State Employees
State Employees
Concerned advocates and community organizations called on Governor Ned Lamont to expand mental health and addiction supports in order to meet the growing demand for these critical services in Connecticut.
In a press conference held at Blue Hills Hospital on Wednesday, frontline workers encouraged Governor Lamont to make structural investments in mental health that address the spiking opioid overdose mortality rates and other conditions aggravated by the loss and isolation due to the COVID-19 pandemic and its ensuing economic hardship.
“No matter what time it is and no matter where you are in Connecticut, you deserve a chance to talk to someone, you deserve access to a program when you are ready to receive help. We can build a mental health support system that meets those needs. We can build a mental health support system that shows you that you are not alone,” said Betsy Eakins, licensed clinical social worker at the Capitol Region Mental Health Center with 33 years of experience. “We are in the business of offering hope to those who too often have fallen victim to a broken system and forgotten promises. We stand with you and we ask everyone to stand with us and support our critical mission here in Connecticut.”
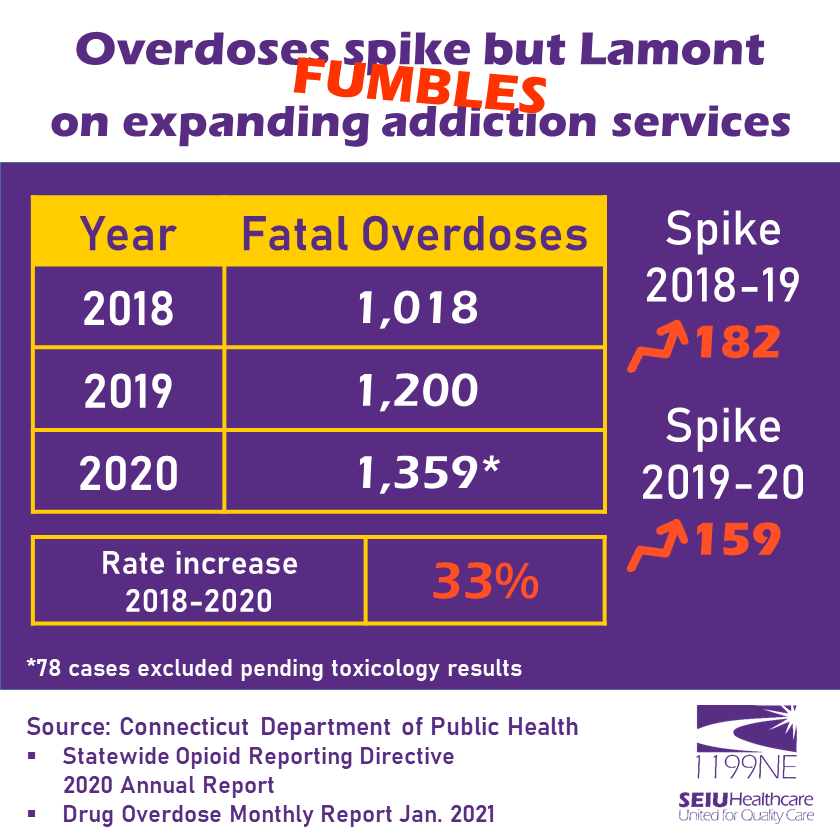
From 2018 to 2020, accidental overdose deaths spiked by 33 percent, from 1,018 fatalities to 1,359 according to recent reports by the Department of Public Health, with 78 cases still pending toxicology results for 2020. If this trend continues and no further investments are made in programs like the mobile crisis unit, accidental overdose deaths could nearly double by the end of fiscal year 2023.
“The COVID-19 pandemic highlighted the existing mental health crisis in Connecticut and throughout the country. People with mental health issues have shared with us that their conditions have been exacerbated by the pandemic.
The need to respond to people experiencing mental health issues has never been greater,” said Lisa Winjum from the National Alliance on Mental Illness Connecticut.
“The stress, uncertainty, and isolation of the pandemic is taking a toll on all of our mental health and the media attention to the crisis is raising awareness about maintaining mental wellness, increasing the demand for the services that NAMI Connecticut and other nonprofit organizations provide. The Governor’s budget proposal doesn’t meet the urgent needs of this moment. We must invest in mental health services, including desperately needed investments in mobile crisis response.”
Incoming calls for support to the Capitol Region’s mobile crisis unit have tripled since the start of the COVID-19 pandemic. Workers and organizations providing support are advocating for a mobile crisis unit that can respond to calls for help 24 hours a day and 7 days a week.
“When we talk about the pandemic, we talk about it in terms of mobilizing as if we were mobilizing for war: the Defense Production Act, bringing all the resources of government to bear to fight the battle. But if our nation were at war we wouldn’t just mourn those lost. We would care for the wounded. And there are wounded here with us. And they deserve our care. This is not a time to step back, not to stay steady, but to put more resources into this recovery,” said Hartford Mayor Luke Bronin as he acknowledged the heroic work of mental health professionals.
“Because if we really, really mean it when we talk about an ‘inclusive recovery’, when we talk about ‘building back better’, when we talk about ‘not returning to the way things were’ but building a ‘new normal’, that’s what it means. It means identifying issues of profound consequence in our communities and tackling them with the seriousness and the resources that they deserve.”
As of late January 2021, the Department of Mental Health and Addiction Services reported that there were 118 individuals on the waitlist for services at Connecticut Valley Hospital.
“If an addict calls us and asks us for a bed, they are not going to wait for us if we can’t get them in right at that moment. The services we provide through DMHAS are immediate. Addicts are calling us in need of beds. We need funding to expand available beds so addicts can get the help they need immediately,” said Victor Rodriguez, a former addict who had an opportunity to rehabilitate and current certified addiction counselor working at DMHAS since 1989.
Making investments in mental health and addiction services creates wealth and wellness in underserved communities by fostering productive lives who can make contributions to the community rather than becoming a burden.
“Connecticut must save lives and begin closing the racial and economic wealth gaps by expanding mental health and addiction services. Every community in our state has suffered the consequences of Connecticut investing too much in incarceration at the expense of services that increase health and opportunity,” said Claudine Fox, interim public policy and advocacy director for the American Civil Liberties Union of Connecticut. “Access to mental health services shouldn’t depend on how much money you have or what your zip code is. The question isn’t how Connecticut can afford to expand mental health and addiction services, but how our state can afford not to.”
With such a heavy toll on mental health reflected in every county in Connecticut and across all races, advocates are calling for compassion and state action to prevent more harm.
“This is no time for business as usual. This is no time for austerity budgeting. This is the time for strategic, compassionate investments in Connecticut’s people,” said Rev. Joshua Pawelek from the Unitarian Universalists Society East. “Invest in health care, in K-12 and higher education, in affordable housing, in cities and towns, in mental health resources, in addiction services, in suicide prevention. Invest in programs that will truly serve struggling communities, low income communities, people of color communities, immigrant communities. Invest so that Connecticut’s most vulnerable communities can stop struggling and start thriving.”
“I witness what happens every day not only at work but also in my local communities. The state must consider expanding services to our communities and clients who are desperately in need of addiction services. It’s a matter of life and death,” said Darrell Coxson, certified addiction counselor with 19 years of experience at Blue Hills Hospital.
“The services that we provide for inner city communities are predominantly services for people of color. We need to expand these services, not cut our resources.” “We must fully fund essential services and hire to fill the over 620 vacant positions in DMHAS.
Unlike the bailout following the Great Recession, it’s time for a recovery that prioritizes the needs of the everyday people,” said Rob Baril, president of District 1199, SEIU, the New England Health Care Employees Union. “It’s time for a recovery that funds public services. It’s time for a recovery that invests in a robust, equitable, and expanded health care infrastructure—because the coronavirus has exposed what happens when society does the opposite.”
Recorded Livestream Video:
Media Contact: Pedro Zayas, pzayas@seiu1199ne.org, 860-830-2478
District 1199, SEIU, New England Health Care Employees Union