Federal workplace safety inspectors are investigating the death or hospitalization of at least three Connecticut elder care workers due to complications from COVID-19.
The investigations come as union officials say at least six unionized nursing home employees have died from coronavirus.
Since late April, the federal Department of Labor has opened investigations at three elder care facilities in Connecticut: Senior Philanthropy of Milford B (aka Golden Hill Rehab Pavilion), Wintonbury Care Center LLC (aka Touchpoints at Bloomfield) and The Linden at Woodbridge.
All three investigations are categorized by the Occupational Safety and Health Administration (OSHA) as “fatal or catastrophic.” A spokesperson for the agency said Thursday such investigations are conducted when an employee death results from a work-related incident or exposure. This category also includes hospitalizations as the result of a work-related incident.
The agency declined to comment on the three open cases.
Getting a definitive tally of nursing home worker deaths in Connecticut is difficult. Employees can sometimes work at several centers, and the state doesn’t report coronavirus testing or case numbers for elder care employees.
“We are heartbroken to confirm that an employee at The Linden At Woodbridge who tested positive for COVID-19 passed while receiving care at a local hospital,” Michael Juno, vice president of East Coast operations at Leisure Care, which manages the facility, said in a statement. “We offer our deepest condolences and support to our employee’s family and loved ones during this difficult time.”
Juno said the company implemented infection prevention plans at the assisted living facility beginning on March 4.
“When the first positive COVID-19 case at The Linden at Woodbridge was confirmed on April 6, we immediately notified all community members and implemented heightened procedures as well as consistent screening and testing,” Juno said.
OSHA opened an investigation into the worker’s death on May 11, and federal records indicate it remains open.
“We are fully cooperating with the inspection and have supplied OSHA with all requested materials,” Juno said.
At Touchpoints, federal inspectors from OSHA opened an investigation into a worker’s death on April 22.
David Skoczulek, a spokesperson for iCare Health Network, which manages the facility, confirmed the death in a statement but declined to comment on the fatality or the OSHA investigation.
The third facility, Golden Hill Rehab Pavilion, did not respond to requests for comment.
OSHA’s Bridgeport office opened an investigation into that facility on May 11. This week, state officials cited Golden Hill for a separate violation, alleging it failed to properly notify conservators when a patient died from coronavirus. The facility, in a response to the state Department of Public Health (DPH), said it “does not agree with the findings.”
Meanwhile, state union officials have confirmed six deaths of nursing home employees. The deceased employees worked at Chelsea Place, Kimberly Hall North, West River Rehab, Trinity Hill, Parkville Care Center, and Long Ridge Stamford, according to Pedro Zayas, a spokesperson for SEIU 1199.
As Worker Deaths Mount, Testing For Employees Grows Slowly
Since Gov. Ned Lamont declared public health and civil preparedness emergencies in early March, elderly residents of nursing homes have been hard hit by COVID-19.
Out of the state’s more than 3,500 deaths, DPH records indicate more than half the people who died were residents of nursing homes and assisted living facilities.
Lamont’s administration has said it is working to prioritize coronavirus testing for nursing home residents. But testing for staff has been slower to roll out, the administration said earlier this week.
“That’s a population that we hope to test on a more repetitive basis,” said Josh Geballe, Lamont’s chief operating officer. “We are a little frustrated by how long it’s taking to get the staff testing ramped up.”
Matthew Barrett, president of the Connecticut Association of Health Care Facilities, a trade and advocacy organization for skilled nursing facilities, said Thursday he anticipates guidance from state officials on employee testing “within a week.”
Barrett said the “optimal strategy” for containing the spread of COVID-19 at nursing homes would be to test residents and staff simultaneously. But that’s a lot of tests — more than 50,000, according to Barrett’s estimate. Lab capacity and supply issues have hindered testing that many people for months.
But Barrett said that as the state builds its testing capacity, rolling out tests for staff across Connecticut all at once could present another problem: not enough workers.
“Given the CDC guidance … that nursing home employees who test positive won’t be able to work for at least 10 days, we are recommending an incremental approach,” Barrett said.
“We believe those staffing shortages could be as harmful or more harmful than delays in testing nursing home employees,” Barrett said. But he said facilities that think they have the readiness to test both should do so.
“We support employee testing not just for the very good reason of assuring for the protection and safety of nursing home employees, but also for their families,” Barrett said. “We also support it because … nursing home employees who show no signs of having the virus could very potentially be having it and be transmitting it in the building.”
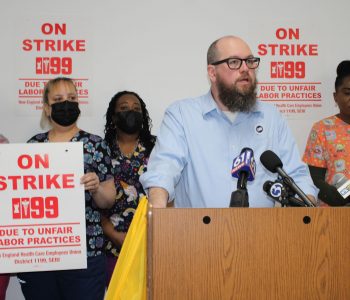
Jesse Martin, a vice president at SEIU 1199, said Thursday that the Lamont administration has yet to present his union with a comprehensive plan about coronavirus testing.
“We haven’t seen anything in writing, or any conversations that I’ve been a party of, to talk about a regime of testing moving forward,” Martin said. “None of that prospective planning has happened from DPH or even the CDC [Centers for Disease Control and Prevention].”
“And so we’re having a lot of nursing home operators have a ton of different policies and procedures, and it’s causing a lot of confusion in our workplaces,” Martin said.
One result of that confusion, Martin said, is the current piecemeal approach to COVID-19 testing for elder care employees.
“I would say that it’s spotty at best,” Martin said Thursday. “It depends on the employer. It depends on if the employer is getting tests through the private marketplace to bring in.”
“It’s a public health issue,” Martin said. “When workers in nursing homes get sick, they don’t live in the nursing home … they bring that virus home with them and become vectors in our communities.”